Waist Size, Blood Pressure, Blood Sugar, and Heart Health!
How Waist Size, Blood Pressure, Blood Sugar, and Heart Health Are All Connected!
Your waistline is not just about appearance — it is one of the strongest signals of future heart health and diabetes risk. When the waist begins to increase, blood pressure, blood sugar, and heart risk usually follow quietly but steadily, often without obvious symptoms. The reassuring truth is that small changes in waist size can bring surprisingly large benefits to overall metabolic health.
***
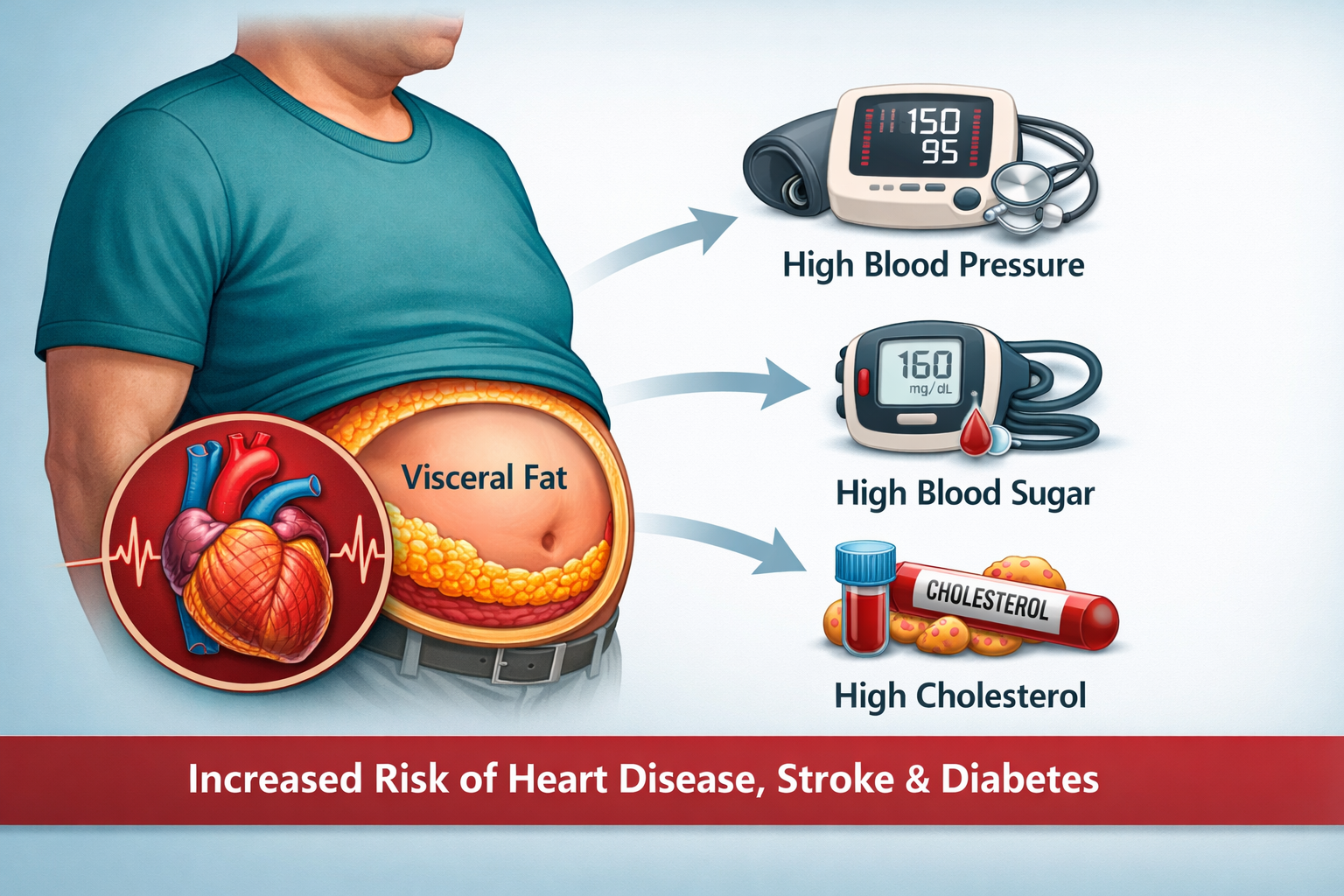
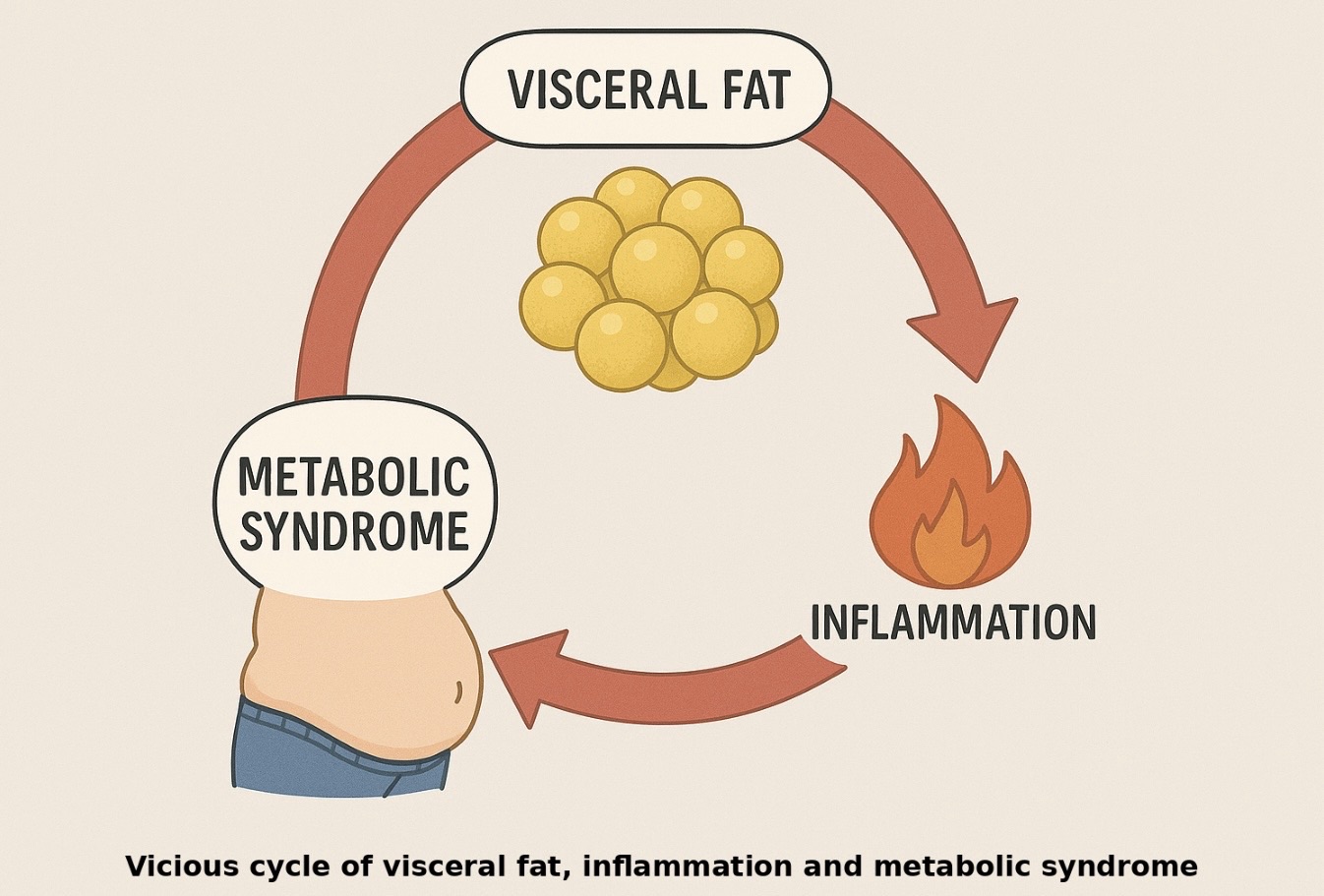
When the Waist Increases: Impact on Blood Pressure, Cholesterol, and the Heart
As the waist size increases, fat accumulates deep inside the abdomen and begins to affect the heart and blood vessels. This abdominal fat raises blood pressure by increasing stress hormones and making the body retain more salt and water. At the same time, it disturbs blood fats — triglycerides rise, good cholesterol falls, and LDL cholesterol becomes more harmful to the arteries. Even when total cholesterol numbers appear acceptable, the quality of cholesterol worsens. Over time, these changes quietly damage blood vessels and significantly increase the risk of heart disease.
***
When the Waist Increases: Impact on Insulin, Blood Sugar, and Diabetes Risk
An increasing waistline also interferes with how the body handles sugar. As abdominal fat builds up, the body becomes resistant to insulin, forcing the pancreas to produce more insulin to keep blood sugars under control. This leads to persistently high insulin levels, rising fasting and post-meal blood sugars, and gradual increases in HbA1c. In the early stages, sugar reports may show only mild abnormalities, but the underlying problem is already active. Over time, this process progresses from normal sugars to pre-diabetes and eventually to type 2 diabetes.
***
When the Waist Reduces: Benefits for Blood Pressure, Cholesterol, and the Heart
The good news is that reducing waist size has a powerful and often rapid effect on heart health. As abdominal fat decreases, blood pressure begins to settle, salt and water balance improves, and blood vessels become more relaxed and flexible. Triglycerides fall, good cholesterol improves, and LDL cholesterol becomes less damaging to the arteries. These benefits often appear even before major weight loss is seen on the weighing scale, translating directly into a lower risk of heart disease.
***
When the Waist Reduces: Benefits for Blood Sugar and Diabetes Prevention
Waist reduction also helps restore healthy insulin action. As abdominal fat reduces, insulin levels fall, fasting and post-meal blood sugars improve, and HbA1c gradually comes down. Many people notice better sugar control within weeks of simple lifestyle changes, even before large changes in weight occur. This improvement can halt or even reverse pre-diabetes and significantly reduce the risk of developing type 2 diabetes.
***
In short:
Reducing waist size is not about looking thinner; it is about preventing heart disease and diabetes before they start. You don’t need drastic diets — small, consistent habits that shrink the waist, such as regular walking and post-meal movement, can quietly reverse rising blood pressure and blood sugar and protect long-term health.
Also read the article ‘Abdominal Obesity’, Diabetes And Heart Disease’ on this website.